Scientists Find Alzheimer’s Earliest Trigger—And Block It Before Symptoms Start
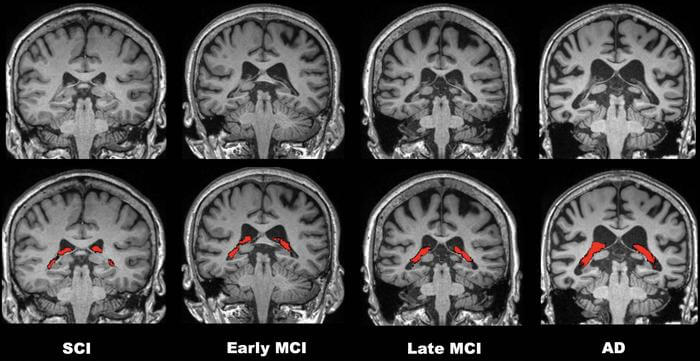
Alzheimer’s disease spends decades quietly dismantling the brain before a single memory slips. Northwestern University researchers have now pinpointed what appears to be the disease’s opening move: a toxic sub-species of protein clusters that ignites inflammation long before confusion or forgetfulness begin.
The discovery, published in Alzheimer’s & Dementia, comes with something even more promising: an experimental drug that stopped the damage in its tracks when given before symptoms appeared.
The culprit is a specific type of amyloid beta oligomer, dubbed ACU193+. While researchers have long known that amyloid plaques litter the brains of Alzheimer’s patients, these smaller, soluble clusters move through tissue far more freely and cause considerably more harm. The team discovered that ACU193+ first appears inside stressed neurons, then migrates to star-shaped brain cells called astrocytes. Once attached, it acts like a spark landing on dry grass—triggering a spreading inflammatory response that damages synapses and accelerates neurodegeneration.
Using 5xFAD mice, which rapidly develop Alzheimer’s-like pathology, scientists detected the ACU193+ subtype in the subiculum—a memory-critical brain region—as early as eight weeks of age. That’s months before the animals show any behavioral problems. The abundance of these oligomers correlated directly with neuron degeneration, suggesting they’re not just bystanders but active drivers of the disease’s earliest phase.
“Alzheimer’s disease begins decades before its symptoms appear, with early events like toxic amyloid beta oligomers accumulating inside neurons and glial cells becoming reactive long before memory loss is apparent,” Daniel Kranz, the study’s first author, explains.
An Experimental Drug With Striking Results
The researchers tested NU-9, a small-molecule compound originally developed to block toxic protein buildup in other neurodegenerative diseases. Mice received daily oral doses for 60 days, starting before symptoms emerged. The effects were dramatic: NU-9 sharply reduced reactive astrogliosis, the inflammatory state that marks early cognitive decline. It also cleared the ACU193+ clusters and lowered levels of pTDP-43, a protein linked to severe memory impairment across multiple brain diseases.
The drug’s impact wasn’t confined to a single brain region. Improvements appeared throughout the areas studied, suggesting NU-9 has a broad anti-inflammatory effect rather than targeting one narrow pathway. Senior author William Klein described the outcome as “stunning,” noting the drug’s remarkable effect on neuroinflammation at the disease’s earliest stage.
What makes this approach different is its timing. Most Alzheimer’s treatments have focused on clearing the large, visible plaques that accumulate late in the disease—often after neurons are already dying. NU-9 targets the instigator, not the aftermath. One researcher compared it to prescribing statins: elevated cholesterol doesn’t cause immediate symptoms, but lowering it early prevents heart attacks years later. Similarly, NU-9 could potentially be given when blood-based biomarkers signal Alzheimer’s risk, long before memory problems begin.
The Second Subtype and What Comes Next
The team also identified a second oligomer subtype, NU4+, which appeared later and formed denser deposits. But it was ACU193+ that correlated most closely with the first signs of trouble, making it the more urgent target for early intervention. This distinction matters for drug development. Stopping the spark is more effective than fighting the fire once it’s already spread.
The researchers emphasize that human trials are still needed. They’re now testing NU-9 in more complex animal models that better reflect human aging, and following treated animals over longer periods to see if neuron health and memory are preserved. With new blood tests capable of detecting Alzheimer’s biomarkers years before dementia, the combination of early diagnosis and prophylactic treatment could fundamentally change how the disease is managed.
Instead of treating devastating end-stage symptoms, medicine may soon intervene at the moment when the brain is most vulnerable—not when memory fails, but decades earlier, when the first toxic signals begin to spread.
Alzheimer’s & Dementia: 10.1002/alz.70968
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!